New genetic therapy could be a gamechanger for MND and frontotemporal dementia
Macquarie University neuroscientists have developed a single-dose genetic medicine that has been proven to halt the progression of both motor neurone disease (MND) and frontotemporal dementia (FTD) in mice – and may even offer the potential to reverse some of the effects of the fatal diseases.
First published by Macquarie University
Macquarie University neuroscientists have developed a single-dose genetic medicine that has been proven to halt the progression of both motor neurone disease (MND) and frontotemporal dementia (FTD) in mice – and may even offer the potential to reverse some of the effects of the fatal diseases.
It may also hold opportunities for treating more common forms of dementia, such as Alzheimer’s disease, which is the second most common cause of death in Australia after heart disease.
The new treatment, dubbed CTx1000, targets pathological build-ups of the protein TDP-43 in cells in the brain and spinal cord.
Cells like neurons produce TDP‑43 naturally, and it is important for their healthy function. Under certain conditions, it accumulates in the wrong part of the cells, clogging them and preventing them from working properly.
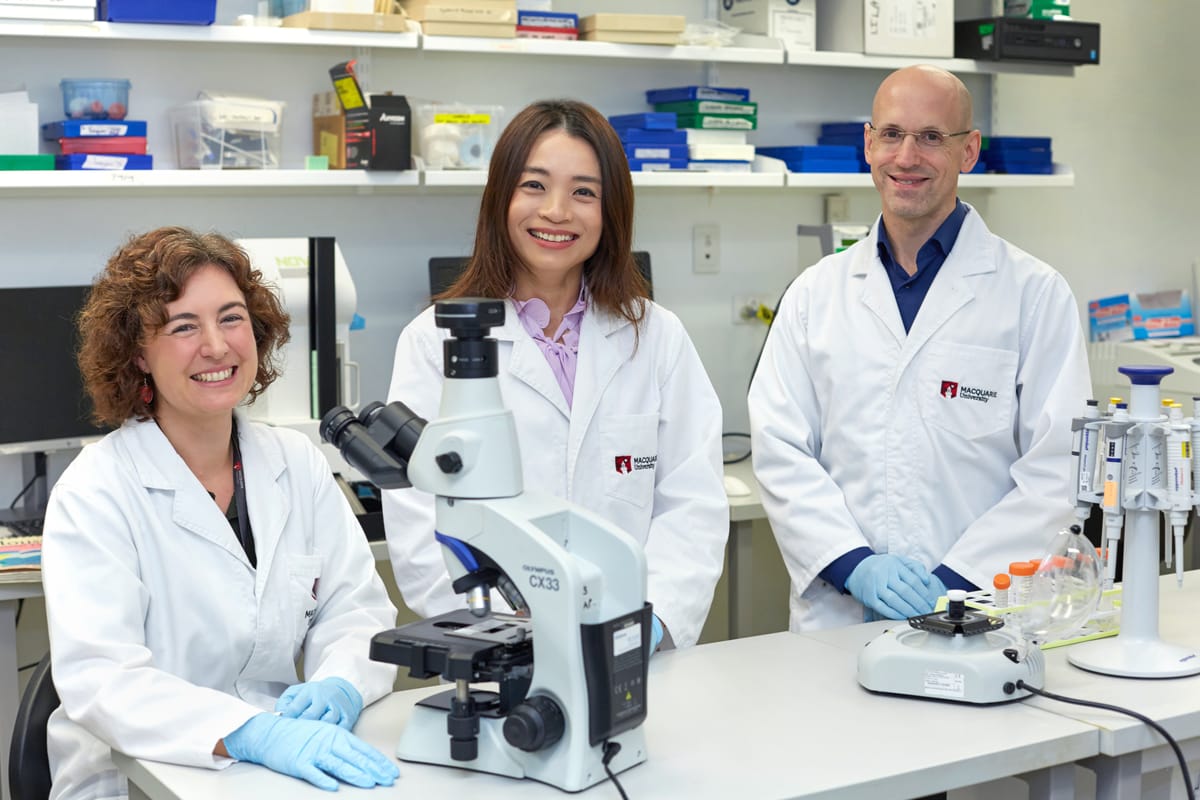
For the past 15 years, a Macquarie University research team led by Professor Lars Ittner has been looking for the causes of this pathological build-up of TDP-43, along with ways to clear the blockages and prevent them from forming in the first place.
The team’s latest findings are published in prestigious international neuroscience journal, Neuron.
Professor Ittner says their research has furthered their understanding of MND and FTD and their causes.
“We discovered for the first time that where there is pathological TDP-43, there is also an increase in a second protein, 14‑3‑3,” he says.
“The two proteins interact, resulting in these build-ups in the cells.
“From this, we were able to isolate a short peptide that controls this interaction, and that’s what we used to create CTx1000.
“When we administered it in the lab, it dissolved the build-ups, tagging TDP-43 proteins for recycling by the body, and prevented new ones from forming.
“Importantly, CTx1000 targets only pathological TDP-43, allowing the healthy version of the protein to be produced and go about its work unhindered.”
This makes CTx1000 incredibly safe, and Professor Ittner says they have seen no adverse effects in their studies.
“We have great hopes that when this progresses to human trials, it will not only stop people from dying from both MND and FTD, but even allow patients to regain some of the lost function through rehabilitation.”
Professor Yazi Ke, lead author of the new paper, says the milestone is particularly exciting for her because the original discovery was made in her early postdoctoral days.
“This spans more than a decade of work, and goes from discovery all the way through to a potential treatment,” she says.
“In lab conditions, we saw CTx1000 stop MND and FTD from progressing even at very advanced stages, and resolving the behavioural symptoms associated with FTD.
“We have great hopes that when this progresses to human trials, it will not only stop people from dying from both MND and FTD, but even allow patients to regain some of the lost function through rehabilitation.”
Research Fellow Dr Annika van Hummel says they covered a variety of mutations in the TDP genes during lab testing.
“We wanted to prove beyond a doubt that this would work in different situations, and it resulted in clear improvements in both symptoms and brain pathology,” she says.
“The fact that it was effective both before and after the onset of symptoms makes it particularly exciting.
“While we are initially concentrating on MND and FTD, but about 50 per cent of cases of Alzheimer’s also show TDP pathology, so it’s possible that in the future this treatment could be translatable to other neurodegenerative conditions.”
A desperate need for treatment options
Also known as amyotrophic lateral sclerosis (ALS), MND causes the progressive loss of the neurons that allow the brain and spine to communicate with the muscles.
In its early stages, patients experience muscle weakness, but as the disease progresses, they gradually lose the ability to walk, speak, swallow and breathe unaided.
Most people with MND die within two to five years of diagnosis.
FTD is one of the rarer forms of dementia, but it is the second-most common form in people younger than 65. Actor Bruce Willis was diagnosed with FTD in 2023.
It does not always have obvious physical symptoms, but it results in cognitive decline coupled with behavioural symptoms including anxiety, loss of inhibition, personality change and impaired judgment. Patients may live for more than 10 years after diagnosis, but it is ultimately fatal.
While there is a genetic therapy showing promise for one form of familial MND, there are few treatments available for the sporadic MND that makes up 90 per cent of all cases.
“This new research is incredibly promising in slowing the progression of MND and FTD for the vast majority of our patients.
Of those, the most effective can only extend a patient’s life by up to five months. All require frequent doses, and some come with side effects that are difficult to cope with.
There is currently no treatment for FTD.
Macquarie University Professor of Neurology, Professor Dominic Rowe, is one of Australia’s leading MND clinicians and researchers.
“I am currently treating more than 200 people with MND, but only five of them with a specific type of familial MND are currently able to access genomic therapy,” Professor Rowe says.
“Treatment like that doesn’t exist for anyone else. For most patients, all we can do is provide good quality, multidisciplinary care.
“This new research is incredibly promising in slowing the progression of MND and FTD for the vast majority of our patients.
“I’m extremely hopeful that it will soon be available to our patients at the Macquarie University Hospital MND Clinic.”
The high cost of research
Professor Ittner and Professor Ke hope to be able to begin in-human trials of CTx1000 within two years, and they have already received a pre-clinical grant of $1.2 million from FightMND to assist with the process.
The therapy is one of the key discoveries being championed by Celosia Therapeutics, a Macquarie University spin-out company formed in 2022 to help bring groundbreaking work of the University’s neuroscientists from the lab to patients.
Unfortunately, testing new therapies and bringing them to waiting patients is incredibly expensive – in this case, the cost is an estimated $22 million to get to human trials.
Celosia Chief Executive Officer, Dr Brenton Hamdorf, is actively seeking investment to facilitate CTx1000 to progress to clinical trial stage.
“There is such a desperate need for new drugs for neurodegenerative diseases like MND, and this is an exciting new therapeutic with enormous potential,” Dr Hamdorf says.
“MND is difficult to diagnose because there is no conclusive test. It’s a process of elimination that can take up to 12 or 18 months, by which time, the disease has progressed significantly.
“We have the potential for CTx1000 to be a one-shot treatment that can help people even at late stages of the disease, then it would quite literally be a light at the end of the tunnel that patients and their families just don’t have now.”
This research was funded by grants from the National Health and Medical Research Council and MND Australia.