Calls for more accurate testing to prevent antibiotic allergies in children
Research from Edith Cowan University (ECU) has highlighted the need for children with a suspected antibiotic allergy to be fully assessed by drug allergy services.

First published by Edith Cowan University
Research from Edith Cowan University (ECU) has highlighted the need for children with a suspected antibiotic allergy to be fully assessed by drug allergy services.
ECU PhD student Ms Annabelle Arnold noted that in children, a label of antibiotic allergy is commonly acquired during an illness, when underlying symptoms from the illness could present as an allergy to antibiotics.
These symptoms could include anything from mild rashes and some itching, through to hives and ultimately, anaphylaxis.
"We know that around 90% of suspected antibiotic allergies are inaccurate. Children who present with these milder symptoms are often actually experiencing symptoms of the infection that they are being treated for, and this is often misconstrued as an allergic reaction," Ms Arnold said.
She noted that a misdiagnosis of antibiotic allergy could result in the unnecessary avoidance of key antibiotics, delayed treatment for children suffering from illness, and longer hospital stays. This line of treatment could continue into adulthood, putting a strain on both the patient and the medical system.
"An antibiotic allergy label has a significant impact on the clinical care of children that come into hospital, and this is exacerbated when the child comes in under the microbial stewardship programme of the hospital, where appropriate antimicrobial management is paramount, and where we have evidenced increased alternative prescribing and longer hospital stays for children with an antibiotic allergy label”.
"Adults that have a perceived antibiotic allergy are often prescribed alternative reserved antibiotics, which result in some illnesses becoming resistant to antibiotics. These patients also have higher intensive care admissions. So, this antibiotic allergy label goes with you throughout your healthcare journey."
Instead, Ms Arnold has urged children with a suspected antibiotic allergy to be tested once the child is well enough.
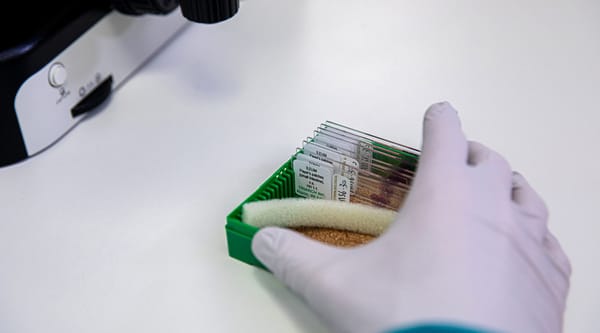
The process of challenging the antibiotic allergy starts with a conversation, Ms Arnold said, outlining the supposed symptoms of the allergic reaction. Skin testing is only done on children with a reported history of a severe reaction. If necessary, a two or three-stage oral challenge is conducted, where children are administered with a dose of antibiotics.
A five-day course is prescribed to rule out any delayed reactions.
"Through our studies, we have found that most reactions occur within the first five days of treatment, rather than immediately after the graded challenges. So, for completeness, we want to be able to present the GP with conclusive proof on any reactions that the antibiotics elicited."